Trauma
The Intersection of Trauma and Eating Disorders
New research shows how trauma therapy helps recovery from an eating disorder.
Posted June 7, 2023 Reviewed by Davia Sills
Key points
- Up to 50 percent of people with eating disorders also have PTSD.
- PTSD complicates ED treatment, yet trauma therapy is not included in most eating disorder recovery programs.
- A real-world study shows how trauma therapy improves recovery for patients with PTSD and eating disorders.
Traumatic experiences, such as sexual or physical abuse, severe bullying, psychological abuse, unhealthy pacing, or accidents, are common among people with eating disorders (EDs). In fact, up to 50 percent of people with EDs also meet the diagnostic criteria for post-traumatic stress disorder (PTSD)1, and researchers think that ED behavior may, in some cases, be a maladaptive way of responding to the long-lasting effects of a traumatic experience2. Somehow, trauma changes the way we relate to our bodies, and our bodies become a tool for dealing with our trauma. This means that in order to treat EDs effectively, we may also need to address an underlying trauma.
Surprising to many, residential treatment for EDs typically does not include targeted trauma therapy. I recently interviewed Dr. Molly Perlman, a psychiatrist and chief medical officer at a leading eating disorder treatment center, about her team's recent study testing how one type of trauma therapy influenced ED recovery in a residential treatment setting3.
What is PTSD-ED, and why should we pay more attention to trauma in EDs?
PTSD-ED refers to people that meet the diagnostic criteria for both PTSD and one or more EDs. Compared to people with ED that now have PTSD, PTSD-ED patients tend to have an earlier onset of ED behaviors, more severe ED symptoms and are more likely to drop out of treatment1. If they do complete treatment, they are more likely to relapse after discharge1. Even if patients do not meet the full criteria for PTSD, previous trauma is a risk factor for developing EDs and worsens ED symptoms and treatment outlook.
.jpg?itok=6kdSzscg)
Similar to other studies, Dr. Perlman and her team found that around 50 percent of their adult clients with EDs also had PTSD, and this was also the case for 38 percent of the adolescents. Shockingly, almost no research is testing what we can do to improve treatment outcomes for this large population of ED patients. To Dr. Perlman, it is clear that we need to address the trauma in order to successfully treat the ED. So that’s what her and her team did.
Why is trauma therapy not a standard part of ED treatment?
I first wanted to understand why trauma therapy is not already a standard part of ED treatment. Apparently, many professionals, including Dr. Perlman, were trained to avoid addressing previous traumas during ED treatment. “I was trained not to open “the trauma box.” They told us not to touch a patient’s trauma during therapy because it would only worsen the ED symptoms or lead to relapse after discharge… but research, including ours, is now starting to show that this assumption is wrong and that we have to address the trauma concurrently with the ED.”

Dr. Perlman points out that one of the major challenges with ED patients is that they tend to drop out of treatment programs, and a common concern is that they may drop out in response to a reactivated and unprocessed trauma that triggers relapse into disordered eating or self-harm. This concern has served as one of the major reasons for excluding trauma therapy during ED treatment. However, when clients dropped out of the combined trauma and ED residential treatment program prematurely, they still showed improvements in several ways. Said differently, we might not need to worry about PTSD-ED clients receiving incomplete trauma therapy.
How does trauma therapy improve ED treatment?
Dr. Perlman’s team implemented a well-known type of trauma therapy, called Cognitive Processing Therapy (CPT), into their eating disorder treatment regimen. CPT is very similar to Cognitive Behavioral Therapy (CBT), and one of its major advantages is that it is a highly standardized method, meaning that different therapists can follow the same guidelines to achieve the same results. For a large organization, standardized procedures are critical to ensure that all clients receive the same level of care. Scientists have reported that CPT improves outpatient treatment for EDs, but Dr. Perlman’s team has demonstrated that CPT also improves ED outcomes during residential treatment.
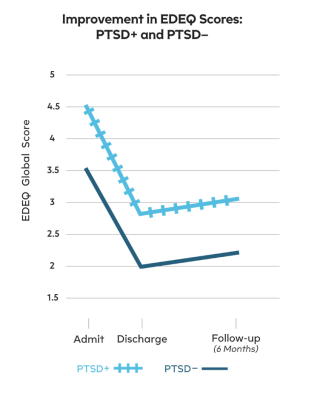
Typically, PTSD-ED patients relapse faster after treatment discharge, but with CPT treatment, they maintained their reduced ED symptoms as well as ED patients without PTSD. Although PTSD-ED patients still had higher symptom severity, these results encourage the idea that addressing preexisting trauma may improve their long-term treatment outcomes.
CPT helps people understand why and how trauma contributes to their ED, and it instills the hope that recovery is possible. When people understand that their ED is tied to their trauma, it becomes easier to let go of the ED as they work through their trauma. In other words, CPT endows people with new coping skills and helps them reconnect with their bodies in a healthy way.
It is commonly said that no one recovers from EDs; you only learn to live with them. I know personally that this is not true. We can recover. Dr. Perlman agrees: “Our clients are so resilient, yet these [EDs] are so tenacious. [Our clients] need treatment to be armed with the tools to combat these negative [ED] thoughts. It is a battle, but we know recovery is possible. With the right treatment, recovery is possible.”
References
1. Day S, Hay P, Tannous WK, Fatt SJ, Mitchison D. A Systematic Review of the Effect of PTSD and Trauma on Treatment Outcomes for Eating Disorders. Trauma Violence Abuse. 2023 Apr 26:15248380231167399. doi: 10.1177/15248380231167399. Epub ahead of print. PMID: 37125723.
2. Trottier K, MacDonald DE. Update on Psychological Trauma, Other Severe Adverse Experiences and Eating Disorders: State of the Research and Future Research Directions. Curr Psychiatry Rep. 2017 Aug;19(8):45. doi: 10.1007/s11920-017-0806-6. PMID: 28624866.
3. Brewerton TD, Gavidia I, Suro G, Perlman MM. Eating disorder patients with and without PTSD treated in residential care: discharge and 6-month follow-up results. J Eat Disord. 2023 Mar 27;11(1):48. doi: 10.1186/s40337-023-00773-4. PMID: 36973828; PMCID: PMC10044735.




