Coronavirus Disease 2019
Cognition and Contagion
How the novel coronavirus can outsmart our behavioral immune system.
Posted April 12, 2020 Reviewed by Gary Drevitch
When Will Restrictions End?
Most Americans currently face substantial restrictions on their daily lives, which governments have imposed as a means for slowing the COVID-19 pandemic. The question for most people, especially for healthy people in serious need of their next paycheck and residing in areas where few people are infected and where, perhaps, far fewer, if any, have died, is “When will the restrictions end?”
In thinking about the question of when to begin easing restrictions, at least two considerations deserve attention.
Balancing Conflicting Concerns
The first of those considerations concerns normative questions. The standard assumption (it may deserve rethinking) is that, inevitably, public health considerations and economic vitality are mostly at cross purposes. The more stringent the restrictions, the more the economy suffers. Conversely, removing the restrictions will free up the economy, but it will also result in far more people dying in both the near term and overall. If this framing of the situation is correct, no ideal answer exists about when to lift the restrictions. Adopting severe measures for a long time might save tens or even hundreds of thousands from dying from the coronavirus, but at some point that would come at the cost of many thousands of deaths, at least, from other causes (including lack of healthcare) and the possibility of both economic stagnation and more deaths for years going forward. A good healthcare system, after all, depends in the long run upon having a solid economy.
A Perfect Storm?
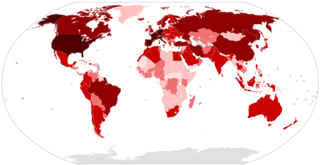
The combination of some characteristics of COVID-19 and the lack of preparedness for such a pandemic raises a psychological consideration. The available evidence suggests that even when they are asymptomatic people infected with the coronavirus can unknowingly transmit the virus to others. Moreover, experts estimate that between a quarter and half of those infected may remain asymptomatic throughout the entire course of their infection. Combined with the fact that, currently, no country in the world can do the number of tests that are needed to identify even most (let alone, all) of these asymptomatic individuals, this is creating a near perfect storm when it comes to people’s intuitions about when to begin relaxing restrictions. And that is true, no matter what trade-off between saving lives and saving the economy any society decides upon.
The Psychology of Contagion
A wide array of evidence suggests that human beings have an evolved psychological repertoire that yields behaviors, which defend against contagious threats. Unlike immunological responses, which are reactive, these behaviors are preventative. The associated affective response is disgust (for example, at hearing someone nearby coughing).
Broadly speaking, this behavioral immune system prompts a wide array of avoidance behaviors in the face of pathogen-connoting stimuli. The operations of such evolved psychological systems rely on a few diagnostic cues rather than a thorough inventory of the available evidence. This means that these systems can make errors.
A Fallible Contagion Management System
With any problem of detection, those errors are of two sorts. These systems can overgeneralize (false alarms), and they can remain blind to unexpected cases (misses). If we automatically avoid people who sneeze because they have allergies, our contagion management system has committed a false-positive error (a false alarm). Allergies are not contagious, but the system leads us to respond as if they are. We are unnecessarily cautious.
False-negative errors (misses), by contrast, are far more dangerous. They arise when the system fails to detect and, therefore, avoid someone or something that is infectious. Over time, organisms possessing contagion management systems prone to misses are less likely to persist, since they would permit contact with some infectious agents.
Because of that perfect storm—that is, because someone with COVID-19 who is asymptomatic will not cue the behavioral immune system and because we lack testing to discover COVID-19 victims who are asymptomatic, no matter what decision is made about the tradeoff between economic and public health considerations, people, who only trust their intuitions or who tout common sense, will be more likely, all else being equal, to make false-negative errors. In his comments about the federal government’s response to the pandemic in an email exchange reported in the New York Times, Dr. James Lawler, an expert in infectious diseases at the University of Nebraska, stated that “We have thrown 15 years of institutional learning out the window and are making decisions based on intuition.”
A recent study from the University of Texas gives some idea of the dangers this may pose. In a summary of that study’s findings, James Glanz and his colleagues show that American counties with only one death from COVID-19 have a better than 50/50 chance of community-spread and an epidemic. Perhaps even more startling is the finding that counties without any deaths so far still have a 9% chance of the same.
References
Schaller, Mark. (2016). The behavioral immune system. In The Handbook of Evolutionary Psychology (second edition, volume 1). D. Buss (ed.). New York: Wiley, pp. 206-24.


