Health
The Tipping Point Toward Mental Health
Can community members rise up to provide mental health care?
Posted April 6, 2017

Last week, I witnessed a community collaboration of minds that may show the path to tackling mental illness as a public health problem in the United States. UT Southwestern and Austin College sponsored a public session with Dr. Vikram Patel and Dr. Madhukar Trivedi, discussing their reverse-Ivory-Tower approach of empowering community members, primary care providers and high school students in early detection and prevention of debilitating mental illness.
What they suggested was not a pill, panacea or a self-aggrandizing methodology for which audience members could pay for a cure. As someone who has managed her own depression/bipolar symptoms for over a decade, researching and reading to arm myself with the best protective tools, the simplicity of what these two men said resonated with all I know. Their approach makes me so excited it is hard to sit in my chair and write. They are democratizing mental health. The power for quantum- shift change in the area of mental health rests not in one institution, method or pill. Change requires a communal effort powered by individuals.
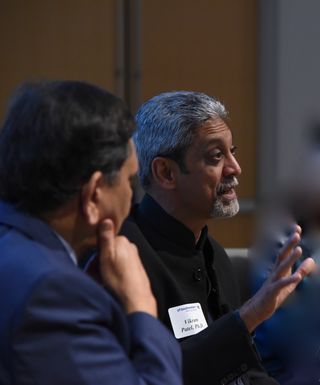
Dr. Vikram Patel came to Dallas last week to receive the well-deserved Posey Award from Austin College. Patel, has become a mental health rock star for this work in India, Nepal, Uganda, Malawi, Zimbabwe, and elsewhere, his approach featured on a TED Talk. He’s formerly from the London School of Hygiene and Tropical Medicine, but has moved to an appointment as The Pershing Square Professor at Harvard Medical School as of early April 2017. Patel’s work outstrips his impressive credentials. As with all great researchers, his humility drives his ability to observe, gather data, and change his assumptions.
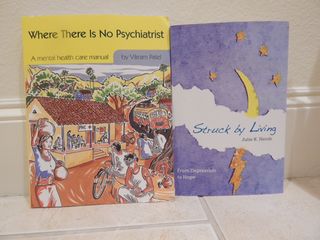
His theory, after over 20 years of research in the field, is this: we need to integrate mental health care into the culture, de-medicalize the principles of psychiatry and psychology, educate, personalize care and empower community leaders who have a passion for mental health to recognize problems and provide a first line level of care. This summer, Patel will release the second edition of his a manual for community leaders, Where There Is No Psychiatrist. The online version of this edition will be available for free and incorporates his years of experience and honing of his theories for real-life applications.
Dr. Patel’s work seemed a natural extension of Dr. Madhukar Trivedi’s work, so I suggested that we host a panel with both Trivedi and Patel. Trivedi, Director of the Center for Depression Research and Clinical Care at UT Southwestern has two major initiatives in Dallas, one with primary care providers and another with high schools. Over the past two years, Trivedi has teamed with 19 primary care practices with a program called VitalSign6. VitalSign6, a software program that works on an iPad, is a depression screen that extends or contracts depending on the answers provided by the patient. VitalSign6 is used at every primary care visit, making mental health a vital measure just like the traditional five vital signs of temperature, pulse, respiration, blood pressure and pain.

In high schools, Trivedi taking a similar approach, first training students about mental health and stress management through the interactive YAM program and then measuring their mental health consistently with a teen version of VitalSign6. YAM was “Americanized” from the Youth Aware of Mental Health, a program developed by scientists from NASP/Karolinska Institutet in Sweden and Columbia University. YAM has had documented success.
The VitalSign6 primary care effort has been in place about a year and a half, already screening about 40K patients. Some of the stats are unsurprising. About 15% of patients screen positive for depression and/or bipolar. The stunner of his research is this, only about 1% of the patients who screen positive need the care of a psychiatrist once the primary physician is trained to manage the patient’s mental health care and is and is partnered with resources in the community to provide psychotherapy, as needed.
What is revolutionary about this? Think about the stark shortage of psychiatrists we have in the medical system. Trivedi suggests that the shortage is not really a shortage, but poor triage and training. “If the primary care physician has the right tools to provide care,” Trivedi asserts, “then only the complex problems go to the specialists.” Considering mental health care hinges on lifestyle management, as does most health, a trained generalist is well equipped to monitor mental health when s/he is helping a patient manage diabetes, blood pressure and/or other ailments.
Patel’s work extends this concept beyond the primary care physician into the community. This is where his brilliance lies. In my experience, so much of managing my mental health is having a supportive community who can help nudge me back to a healthy lifestyle when I don’t sleep enough, pace myself, take medication or practice self-care. If there are non-threatening, trained resources in the community that can provide an educated nudge to center, I can stay out of the doctor’s office even longer.
If you are curious, here is the link to the discussion with Dr. Patel and Trivedi, which I moderated. Out of curiosity, I asked Dr. Patel how he selected these community counselors. “At first we had medical mental health professionals selecting people for listening skills,” he said. That approach lead to mediocre results. Then, he simply put an ad in the paper asking for people who felt called to help with the mental health of their communities. The desire to help proved a better indicator of a better person for the job. He took people with passion and trained them to be more effective in their passion.

As we wrapped up the session, Dr. Patel turned to me and said, “It is clear you are passionate about this.”
I smiled and answered with my usual sarcasm, “Whether I like it or not.” Gotta learn to control that and accept the compliment.
Sometimes I feel crushed by the weight of the problems of mental illness. I attended a funeral of a young man last Friday, 34 years old, brilliant mind, son of a dear friend, so much potential snuffed out by the Grim Reaper of depression. My hope is through the work that Dr. Trivedi and Dr. Patel are doing, we can save lives like his.
We are not there yet, but in the words of the immortal Dr. Martin Luther King, “I’ve Been to the Mountaintop.” Change is coming. Dr. Patel and Dr. Trivedi are leading the way.
For more information about Julie K. Hersh and the newly released edition of Struck by Living, please check out the Struck by Living website.




