Dementia
The Complicated Relationship Between Dementia and Sexuality
Grappling with issues of sex and consent for persons with dementia.
Posted June 18, 2021 Reviewed by Devon Frye
Key points
- Persons with dementia possess the capacity for sexual desire.
- Recognizing the sexuality of a person with dementia assists in the maintaining of personal identity.
- Whether a person with dementia can offer sexual consent is a complicated issue.
- Care facilities must expand their knowledge regarding the sexuality of residents and make informed policy decisions in a team approach.
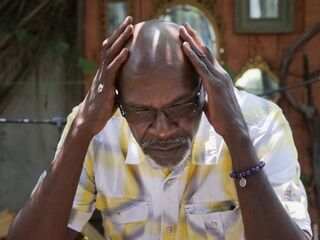
When considering issues of sexuality and dementia, two core and essential questions emerge. First, how does one address the fact that a person with dementia likely has sexual needs? Second, what are the implications of sexual consent in terms of a person with dementia? Both are vital questions that need continued exploration inside and outside of healthcare facilities.
Most commonly associated with Alzheimer’s disease, dementia covers an array of medical conditions that interfere with the daily routines and social life of an individual. Dementia is often marked by difficulties with problem-solving, memory loss, decision-making, and language.
In cases of persons with Alzheimer’s disease, dementia progresses through a series of stages, from mild dementia—where the individual has difficulty with things like short-term memory and forgetting where they put things—to severe decline where they struggle to recognize intimate others, possess severe memory loss, and often exist in a state of confusion. Dementia is frequently associated with elderly persons, but dementia can is not limited to that age group and can strike others, too, depending on the disease or adverse health affiliation.
Are People with Dementia Still Sexual Beings?
All too often, people impose their own assumptions about sexuality on those who are elderly or have health conditions. The same prejudices and stereotypes that label the elderly as non-sexual beings (“They are too old to want sex anymore”) are often attached to persons with dementia (“They are too ill/impaired to want sex anymore”).
This stereotype, as with many stereotypes, is simply untrue. Many elderly people still have active sexual desires, needs, and fulfilling sex lives. The same pertains to persons with dementia. Humans are sexual beings—and this applies to people with dementia, regardless of whether they are elderly or younger.
Many people with dementia still have feelings of the need for comfort and intimacy. It’s part of the foundation of our sexual selfhood. Furthermore, their sexuality contributes to their personal identity. The recognition of their sexuality assists in maintaining a sense of identity for persons with dementia, which is a crucial attachment for them. To suggest that persons with dementia are not sexual beings diminishes their humanness.
Can People with Dementia Consent to Sexual Activity?
Now that we’ve established that persons with dementia are, in fact, sexual beings with the capacity to express sexual desire, the larger, and perhaps more controversial question is whether a person with dementia can consent to sexual activity.
The strict criteria of sexual consent may lean towards “no” if the individual is considered to be incapacitated due to their dementia. Legal precedence in most jurisdictions states that the individual offering consent must possess the knowledge to make the decision, display a reasoned understanding, and demonstrate the ability to make a voluntary decision without coercion (Syme and Steele, 2016). Those who would oppose the idea that dementia patients can offer sexual consent may argue that the person lacks the ability to make a knowledgeable decision due to their condition and is vulnerable to undue influence.
Dementia, however, varies widely in severity, and the condition alone may not automatically mean that a person does not have the capacity to consent to sex. Still, exploitation is always a potential danger for persons with dementia.
Bearing all this in mind, what then can be done for people who have both dementia and sexual needs?
The healthcare system often neglects the fact that persons with dementia have sexual needs and their sexual health is an important facet of their overall well-being. Yet, the debate over consent is an ever-present wrinkle in the discussion, further complicating policy-making and procedures.
The healthcare system is responsible for the care of patients. This includes sexual care. Considerations must be made based on the autonomy of a person to act upon their sexual needs while weighing the potential for sexual exploitation. It continues to come down to that single question: Can a person with dementia give sexual consent, whether it’s with a potential new partner or with a spouse? (Marital rape is possible in cases of dementia, just as it is outside of such cases.)
In one study, in the home setting, 48 percent of men and 18 percent of women living at home with dementia were sexually active (Rector, Stiritz, and Morley, 2020). Another study by Lindau, et al., (2018) found that of people with dementia that were partnered, 59 percent of men and 51 percent of women were sexually active. Professionals in the nursing care system, however, struggle with the issues of consent.
In 2014, Iowa state representative Henry Rayhons was arrested and charged with sexual abuse for having sex with his wife, an Alzheimer’s patient, in her room at a care facility. The facility determined that Mrs. Rayhons did not have the cognitive ability to offer consent. In the resulting trial in 2015, Representative Rayhons was found to be not guilty.
How to Navigate Questions of Consent in Dementia
How exactly does one determine whether a person with dementia can offer sexual consent without disregarding or depriving them of their sexual needs? The first question to consider is in the individual’s ability to express themselves sexually. What exactly is appropriate (who can actually make such a decision)? To whom is the individual sexually expressing themself—is it a spouse or a new interest? Are they able to recognize the person to whom they are expressing themself?
Another problem, according to Syme and Steele (2016), is that health providers have limited knowledge in matters of sexual expression for persons in the later stages of their life. That limited knowledge threatens to further deprive a person of independence in a setting where their independence has already been negatively impacted.
James M. Wilkens recognizes the tension between ensuring sexual autonomy and protecting care facility residents from harm. He suggests that in cases where a person with dementia lacks cognitive capacity, but still wishes to act upon sexual needs, there should be a committee approach to a solution. This is an approach in which Wilkens claims “the resident, the nursing home itself, and the family members convene in an effort to advocate for the resident’s autonomy, dignity, and right of sexual expression while working to minimize harm” (Wilkens, 2015:722). This committee approach may further intrude on an individual’s privacy, but in a setting like a care facility, where residents are sometimes dependent upon considerations by others, the deliberative team effort may prove to be most effective overall. Of course, this is assuming that everyone involved participates in open and transparent discussion without self-serving interests.
It’s a complicated issue. There is no easy answer. On one hand, there is a responsibility to protect a potentially vulnerable individual from harm and on the other, there is the risk of unfairly discarding someone’s autonomy and infringing upon their sexual well-being. Persons with dementia, even advanced dementia, still have the capacity for sexual desires. It’s an important topic ripe for more research and truly supportive policy-making.
References
Lindau, S.T., Dale, W., Feldmeth, G., Gavrilova, N., Langa, K.M., Makelarski, J.A., & Wroblewski, K. (2018). Sexuality and cognitive status: A U.S. nationally representative study of home-dwelling older adults. Journal of the American Geriatrics Society, 66(1), 1902-1910.
Rector, S., Stiritz, S., & Morley, J.E. (2020). Sexuality, aging, and dementia. Journal of Nutrition, Health, and Aging, 24(4), 366-370.
Syme, M.L., & Steele, D. (2016). Sexual consent capacity assessment with older adults. Archives of Clinical Neuropsychology, 31(1), 495-505.
Wilkens, J.M. (2015). More than capacity: Alternatives for sexual decision making for individuals with dementia. Gerontologist, 55(5), 716-723.




