Vagus Nerve
What Happens in Vagus
A major gut-brain link, the vagus nerve can be manipulated for mental health.
Posted September 1, 2022 Reviewed by Hara Estroff Marano
Key points
- The vagus nerve is a primary component of the parasympathetic nervous system and a direct link between the gut and the brain.
- Gut-Brain communication through the vagus nerve involves cell-mediated sensing, microbiota direct signaling, and indirect signaling.
- Manipulation of the vagus nerve via electrical stimulation has been shown effective in the treatment of depression and anxiety.
- Noninvasive vagus nerve stimulation via breath work and targeted probiotics are shown to be effective mood improvement strategies.

By Nicole Cain, ND, MA
The vagus nerve is the 10th cranial nerve, also called the wandering or pneumogastric nerve, and is the longest nerve in the body. It contains bidirectional motor and sensory fibers, afferent fibers carrying information from body tissues to the central nervous system and efferent fibers carrying information from the central nervous system to the rest of the body.1
The vagus nerve originates from the medulla oblongata, the bottommost part of the brain, and encased within fibrous tissue (the carotid sheath), it descends down the neck. At the base of the neck, it splits into the left vagus nerve and right vagus nerve, both of which meet up again at the enteric nervous system (ENS)—the nervous system surrounding the gastrointestinal tract.1
The vagus nerve is a main component of the parasympathetic nervous system, which is responsible for bodily functions when at rest. It is also involved in coordinated communication and regulation of the body’s organs, the central nervous system, and enteric nervous system.2
As a major pathway of the gut-brain axis, preliminary evidence suggests that stimulation of the vagus nerve may be a potential approach to relieving symptoms related to both physical and psychiatric conditions such as post traumatic stress disorder (PTSD), depression, anxiety and inflammatory bowel disease.2 In fact, vagus nerve stimulation through surgically implanted devices is currently prescribed for treatment-resistant depression,3 mood and anxiety disorders, and other conditions associated with inflammation.4
Moreover, in a 2022 report, researchers at Leiden University (Netherlands) demonstrated that non-invasive vagus nerve stimulation reduced emotional reactivity and bias—primary components of depression—compared to control subjects.5
What Happens in Vagus: The Microbiome-Mood Superhighway
The vagus nerve represents an important link between the gut microbiome and mental health.2 Although the gut microbiota communicates with the body’s nervous system via a variety of means including hormonal and immune pathways, the most expedient channel of communicateion with the brain is through vagus nerve signaling.6 This signaling consists of several mechanisms including cell-mediated sensing, direct signaling, and indirect signaling.
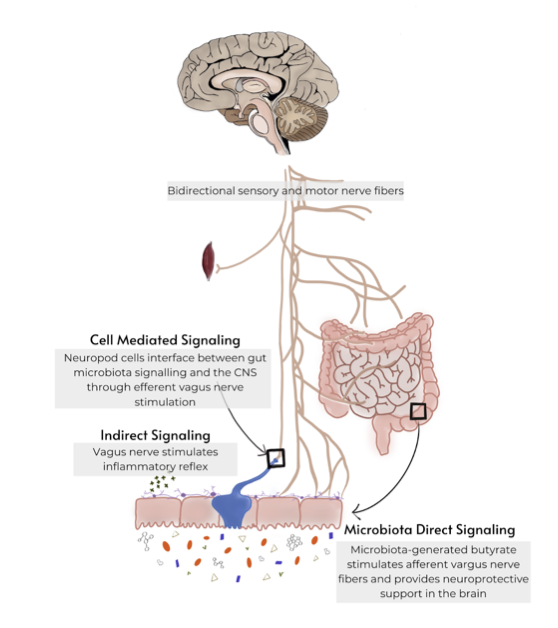
Cell-Mediated Sensing
In cell-mediated sensing, signals from the microbiota are passed to the vagus nerve via intermediary sensing cells. As an example, intermediary sensing enteroendocrine cells (EECs) in the gut interface with vagus fiber cells to carry signals from the microbiota to the enteric and central nervous systems.7
When gut microbes release a compound or metabolite, EECs receive that signal and relay it to the afferent fibers of the vagus nerve. In one example of mood altering neurotransmission, EECs directly release serotonin in the form of 5-hydroxytryptamine (5-HT) and activate 5-HT3 receptors on vagal afferent fibers, which transmit the signal to the central nervous system to modulate mood and cravings.8
Microbiota Direct Signaling
In microbiota direct signaling, gut microbes are able to communicate with the afferent fibers of the vagus nerve directly. For example, butyrate, a short chain fatty acid (SCFA) produced by certain microbiota types such as Firmicutes,9 with the cross-feeding support of Bifidobacteria, can directly stimulate afferent fibers. SCFAs have also demonstrated the ability to maintain the integrity of the blood brain barrier (BBB), providing antiinflammatory, neuroprotective, and brain tissue support.11
Indirect Signaling
Indirect signaling is a process by which signal molecules are able to indirectly affect surrounding cells.12 Vagus nerve afferent fibers stimulate vagal efferent signals via what is referred to as the inflammatory reflex. Vagus efferent fibers are capable of inhibiting the release of certain inflammatory cells in order to manage inflammation, an important component in depression.7,13
Vagus Manipulation: Direct and Indirect
Although direct stimulation of the vagus nerve has been used successfully in the treatment of mood disorders such as major depression, it is complex, expensive14, of limited availability, and even more limited safety and efficacy data.
There are other, nonmechanical ways to stimulate the vagus nerve. Diaphragmatic, or deep and slow breathing (DSB), is a method of deep breathing from the diaphragm in which the exhalation time exceeds inhalation time. When inhaling, the vagus nerve is inhibited, resulting in an increased heart rate, which can lead to an anxious state.15 During exhalation, vagus activity is restored, resulting in a slowing down of heart rate and reduction in the parasympathetic response associated with stress.16 In a 2021 study,17 researchers demonstrated that after just five minutes of DSB, participants showed decreased physiological stress and reported significantly less anxiety.
Targeted microbiome therapies are a newer approach to vagal stimulation. Several species of gut microbes, including strains of L. rhamnosus, B. longum, L. casei, have demonstrated vagus-nerve–mediated mood improvement.18 Identifying a highly effective psychobiotic formulation, however, can be challenging. Formulations backed by specific clinical evidence from human trials offer the most reliable outcomes.
Final Thoughts
As an integral component of the gut-brain axis, the vagus nerve plays a significant role in mood and mental wellness. Fortunately, noninvasive tools like deep breathing and clinically demonstrated psychobiotics offer a safe and effective option to help fine tune the system.19
References
1. Vagus Nerve Anatomy, Medscape 2017. https://emedicine.medscape.com/article/1875813-overview
2. Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain-Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry. 2018 Mar 13;9:44. doi: 10.3389/fpsyt.2018.00044.
3. Aaronson ST, Carpenter LL, Conway CR, Reimherr FW, Lisanby SH, Schwartz TL, Moreno FA, Dunner DL, et al. (2013) Vagus nerve stimulation therapy randomized to different amounts of electrical charge for treatment-resistant depression: acute and chronic effects. Brain Stimul 6:631–640
4. Breit S, Kupferberg A, Rogler G and Hasler G (2018) Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Front. Psychiatry 9:44. doi: 10.3389/fpsyt.2018.00044
5. Johnson, KA., Steenbergen,L. Gut Feelings: Vagal Stimulation Reduces Emotional Biases, Neuroscience,Volume 494, 2022, 119-131, ISSN 0306-4522,https://doi.org/10.1016
6. Fülling, C., Dinan,T., Cryan,J., Gut Microbe to Brain Signaling: What Happens in Vagus…,Neuron,
Volume 101, Issue 6, 2019, 998-1002, ISSN 0896-6273, https://doi.org/10.1016/j.neuron.2019.02.008
7. Bonaz B, Bazin T, Pellissier S. The Vagus Nerve at the Interface of the Microbiota-Gut-Brain Axis. Front Neurosci. 2018 Feb 7;12:49. doi: 10.3389/fnins.2018.00049.
8. Kaelberer MM, Rupprecht LE, Liu WW, Weng P, Bohórquez DV. Neuropod Cells: The Emerging Biology of Gut-Brain Sensory Transduction. Annu Rev Neurosci. 2020 Jul 8;43:337-353. doi: 10.1146/annurev-neuro-091619-022657
9. Venegas D, et al. (2019) Short Chain Fatty Acids (SCFAs)-Mediated Gut Epithelial and Immune Regulation and Its Relevance for Inflammatory Bowel Diseases. Front. Immunol. 10:277. doi: 10.3389/fimmu.2019.00277
10. Rivière A, Selak M, Lantin D, Leroy F, De Vuyst L. Bifidobacteria and Butyrate-Producing Colon Bacteria: Importance and Strategies for Their Stimulation in the Human Gut. Front Microbiol. 2016 Jun 28;7:979. doi: 10.3389/fmicb.2016.00979. PMID: 27446020; PMCID: PMC4923077
11. Silva YP, Bernardi A and Frozza RL (2020) The Role of Short-Chain Fatty Acids From Gut Microbiota in Gut-Brain Communication. Front. Endocrinol. 11:25. doi: 10.3389/fendo.2020.00025
12. Introduction to Cell Signalling, Khan Academy. https://www.khanacademy.org/science/ap-biology/cell-communication-and-c…
13. Miyata S, Ishino Y, Shimizu S, Tohyama M. Involvement of inflammatory responses in the brain to the onset of major depressive disorder due to stress exposure. Front Aging Neurosci. 2022 Jul 22;14:934346. doi: 10.3389/fnagi.2022.934346. PMID: 35936767; PMCID: PMC9354609
14. Fortune Business Insights. https://www.globenewswire.com/en/news-release/2020/02/28/1992626/0/en/V…
15. Ogletree-Hughes, M. et al. Mechanical unloading restores beta-adrenergic responsiveness and reverses receptor downregulation in the failing human heart. Circulation 104, 881–886. https://doi.org/10.1161/hc3301.094911 (2001)
16. Kim, H.-G., Cheon, E.-J., Bai, D.-S., Lee, Y. H. & Koo, B.-H. Stress and heart rate variability: A meta-analysis and review of the literature. Psychiatry Investig. 15, 235–245. https://doi.org/10.30773/pi.2017.08.17 (2018)
17. Magnon, V., Dutheil, F. & Vallet, G.T. Benefits from one session of deep and slow breathing on vagal tone and anxiety in young and older adults. Sci Rep 11, 19267 (2021). https://doi.org/10.1038/s41598-021-98736-9
18. Wang H, Lee IS, Braun C, Enck P. Effect of Probiotics on Central Nervous System Functions in Animals and Humans: A Systematic Review. J Neurogastroenterol Motil. 2016 Oct 30;22(4):589-605. doi: 10.5056/jnm16018. PMID: 27413138; PMCID: PMC5056568




