Chronic Pain
How Rogue Nerves Lead to Migraines, Back Pain, and IBS
Confused nerves can turn up the pain level.
Posted October 9, 2023 Reviewed by Davia Sills
Key points
- Chronic migraines, back pain, and irritable bowel syndrome are types of central sensitization syndromes.
- Central sensitization syndromes (CSS) share the feature of nerve sensitization.
- Nerve sensitization intensifies pain. The pain comes on faster and lasts longer.

What do chronic migraines, back pain, and irritable bowel syndrome have in common? These seemingly unrelated conditions share a common underlying problem—sensitization of the nervous system.
When I was in medical training, the various central sensitization syndromes (CSS) were referred to and treated separately. They affected separate body systems, so the specialist in that body system treated them. There was no relationship seen between someone with a chronic headache disorder and chronic back pain. No relationship between someone with chronic digestive issues and chronic bladder pain. There was no obvious connection between them.
We now understand the conditions do have a connection. A connection that is pivotal to proper treatment.
Sensitization makes nerves more sensitive and reactive to stimuli. More sensitive nerves mean more symptoms, more often. CSS also share the same group of risk factors that lead to their development.
How sensitization starts
Long-term stress is a trigger for sensitization syndromes. The hormones released during the stress response switch on an inflammatory state, which causes inflammation in the nervous system. The inflammation sensitizes the nerves and increases the risk of developing a CSS.
Similarly, high stress worsens symptoms. For example, a former patient, Bryan, developed a headache disorder during an extended period of high stress. Bryan’s nervous system was in overdrive for 10 years, which sparked chronic migraines. His headaches returned each time his stress levels spiked.
Physical injury
Another factor in the development of sensitization syndromes is physical injury. For example, Melissa, a previous patient, suffered a minor back strain. Over months, sensitization developed, perpetuating the pain even after the injury had healed. A joint injury is a common start to sensitization.
As with many medical conditions, some people are genetically predisposed to certain ones. Genetics even affect how you experience pain through genes specific to pain sensitivity! If you have a low pain tolerance, your genetics may be why.
Psychological factors
Sensitization syndromes frequently occur alongside mental health conditions, such as depression and anxiety. Each one affects and worsens the other. The pain disorder increases the risk of depression and anxiety. Anxiety and depression intensify the pain from the disorder. A vicious cycle follows. Sometimes, chronic back pain triggers depression. Sometimes, depression intensifies back pain.
The pain and emotion circuits process pain together, increasing pain perception in the brain. Each condition negatively affects the other. It is not that you are “just depressed” or “just anxious”; depression and anxiety increase the pain perception.
Childhood trauma and abuse are common precursors to certain sensitization syndromes. In the clinic, I recall seeing young women present with whole-body pain, fibromyalgia, and chronic bladder pain. More often than not, these women suffered sexual abuse or trauma as children, abuse that lasted for years.
Abuse may act as the trigger—the injury—initiating the physical changes that lead to sensitization. For example, women who have suffered sexual abuse often develop chronic pain in the bladder or pelvic area, the location of the abuse. The physical trauma causes local inflammation that affects the nerves, resulting in neuroinflammation. Emotional trauma and the stress response cause system-wide inflammation. Neuroinflammation then leads to sensitization and chronic pain.
The brain and nervous system become vigilant guard dogs to keep away repeat trauma. The brain is hyper-responsive to any stimuli it fears may be placing it back in harm's way. Trauma gets embedded in the nervous system.
How the pain progresses
Here’s how sensitization intensifies pain:
- Nerve sensitization is a result of dysfunction in the nervous system.
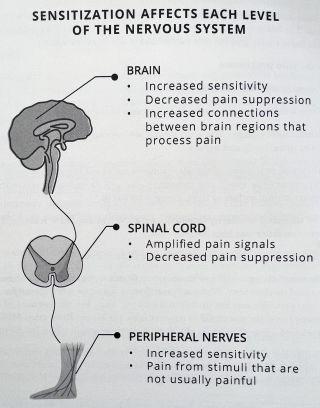
- Sensitization changes how pain signals are processed and perceived in the brain, spinal cord, and nerves.
- Abnormal processing of signals results in increased responsiveness to sensory inputs—like touch and movement—as well as increased reactivity to sensory stimuli, including light, sound, and smells.
- The increased sensitivity intensifies pain. Nerves are more reactive. Pain comes on faster and lasts longer.
- The pain continues, even in the absence of an injury.
The abnormal changes in the nervous system from sensitization do not show up on standard medical tests. Yet, the intensity of the discomfort can make you afraid to move or leave the house. Melissa, who developed chronic back pain, developed a fear of moving, afraid the movement would injure her further.
A closer look
Sensitization develops after an inciting event—an injury, unrelenting stress, or trauma—initiates a cascade of inflammation that spreads to the nervous system, resulting in neuroinflammation. Neuroinflammation sensitizes the nerves and disrupts the normal processing of pain signals.
Think of the brain and nerves like an electrical panel. The panel maintains balance in the system, adjusting its inputs and outputs, creating an even flow of signals throughout the body. Nerve sensitization turns up the signal frequency too high, disrupting the function of the system.
The body has more intense incoming pain signals and loses the ability to turn down those signals. The loss of these two critical processes translates to more pain and less protection, which happens at each level of the nervous system.
Functional MRI is a radiology test that shows what areas of the brain are active during certain tasks, such as picking up objects or feeling pain. It has enabled scientists to see how sensitization changes brain function.
Imaging reveals that those with sensitization process pain differently. They have increased connections between brain regions that process pain and decreased activity in areas that suppress pain. They perceive more pain and have less protection from it.
Bottom Line
Central sensitization syndromes vary in their symptoms, but they all share the feature of nerve sensitization. Sensitization arises from dysfunction in the nervous system. The dysfunction causes more intense pain signals and loss of the body’s ability to turn down the pain signals. The balance is lost like a malfunctioning electrical panel. These changes occur at each level of the nervous system, the brain, the spinal cord, and the nerves. Now that functional MRI provides a visual of brain function, we can see how sensitization changes the way the brain processes pain.
Learn about how to manage sensitization in my book, Sunbreak: Healing the Pain No One Can Explain.
References
Muhammad B. Yunus, “Editorial Review (Thematic Issue: An Update on Central Sensitivity Syndromes and the Issues of Nosology and Psychobiology),” Current Rheumatology Reviews 11, no. 2 (July 2015): 70–85.
Jo Nijs et al., “Nociplastic Pain Criteria or Recognition of Central Sensitization? Pain Phenotyping in the Past, Present and Future,” Journal of Clinical Medicine 10, no. 15 (July 21, 2021): 3203.
Mary-Ann Fitzcharles et al., “Nociplastic Pain: Towards an Understanding of Prevalent Pain Conditions,” The Lancet 397, no. 10289 (May 1, 2021): 2098–2110.




