While it’s commonly believed that clinical depression and other mental health disorders are caused by a “chemical imbalance,” we’ve known for a long time that’s simply not true. There’s now a good deal of evidence that mental health problems are caused by a combination of environmental stressors (such as trauma, infections, brain injury, and lack of sleep) and genetic risk. In the case of clinical depression or anxiety, various stressors lead to chronic over-activation of the sympathetic “fight-or-flight” nervous system and eventually to cortisol resistance, brain inflammation, and a decreased ability of the cells in certain areas of the brain to work efficiently, and a decreased ability of those cells to recover and repair from their daily work. It’s not a lack of serotonin or “chemical imbalance” that causes the problem, it’s an overactive stress response and inability to turn the fight or flight system off.
Anything, then that works to help a clinical depression does not “balance the chemicals” per se, but rather promotes the “rest and digest” side of the nervous system, decreases inflammation, improves anti-oxidant capability in the brain, and improves recovery and repair.
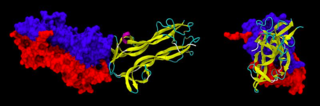
One of the big players in recovery and repair in the brain is our own nerve fertilizer, brain-derived neurotrophic factor, or BDNF. Levels of BDNF are lower in certain regions of the brain during depression, and certain antidepressants and salts, such as lithium, are thought to raise them. BDNF not only helps in recovery and repair in brain injury and depression, but also with just regular tasks such as learning and memory.
We now know that different people have variations in the gene that codes for BDNF. Specifically, one part of the gene can code for methionine amino acid replacing a valine. Those with the methionine substitution in their brain fertilizer, BDNF, have BDNF that moves about the cell differently than those with the valine allele. This is about 1/3 of the population, but the findings are pretty new, and we don't know precisely what it means. These methionine folks have a higher risk of developing depression and have an increased stress response.
What does knowing about brain fertilizer and the genes for it do to help us with diagnosis and treatment? Well, one study showed that exercise is particularly helpful for memory in the methionine allele carriers of the BDNF gene, and another brand new study showed lower markers of inflammation in methionine carriers. Low doses of lithium (far less likely to cause side effects than the standard doses) have also been studied in cognitive impairment and aging and thought to work by raising BDNF. There are even some studies showing that the right diet can affect BDNF (albeit in mice).
In this and my last several blog posts, I’ve been focused not on disorders and symptoms, but on pathology in the brain at a molecular level, looking at abnormalities researchers have found in the genome linked to families with depressive disorders, and then plausible marker genes with clinical interventions we could use in studies today to improve psychiatric treatment by leaps and bounds in the very near future. We know BDNF helps neurons recover, just as fertilizer helps plants grow. We know simple interventions such as a whole foods diet and an exercise program get the brain fertilizer sprinkled around. Researchers and clinicians can work together to see what medications, like lithium or SSRIs might the most helpful for which genetic profiles in folks that don’t respond to less invasive interventions. For the first time, psychiatrists can or are on the verge of being able to explain to patients…here’s where the problem is in the brain, here’s why you are particularly vulnerable, and here’s what we can do to fix it. Exciting times.
Copyright Emily Deans MD
image from Wikimedia Commons of BDNF


