Psychopharmacology
The Fentanyl Death Crisis in America
Medication for reversing overdose is life-saving—if used quickly and correctly.
Posted June 4, 2024 Reviewed by Hara Estroff Marano
Key points
- Fentanyl is a major threat causing overdose deaths in the United States.
- Young people are unknowingly taking fentanyl and dying.
- Fentanyl smoking is contributing to overdose and speedballing deaths.
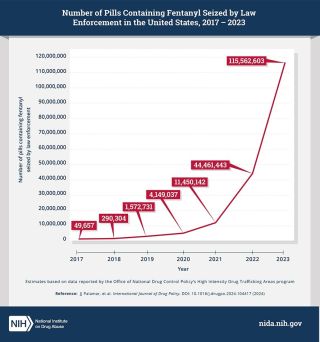
- Government and private agencies are cracking down on illegal fentanyl, but it's an uphill fight.
“It is the deadliest drug threat our country has ever faced.” says Anne Milgram, Administrator, Drug Enforcement Administration (DEA), referring to the threat of fentanyl in the United States. She should know.
We still have record deaths, and that’s after the DEA seized more than 80 million fentanyl-laced fake pills and nearly 12,000 pounds of fentanyl powder so far in 2024 . The fentanyl seizures represent more than 157.6 million deadly doses; 70% of the counterfeit pills contain a lethal dose of fentanyl. Sometimes, the drug is smoked and as with intravenous injection, speeds access to the brain, further endangering users.
The best new prevention approach, the “One Pill Can Kill” initiative led by the DEA, is amplified by the Community Anti-Drug Coalitions of America (CADCA) and other volunteers educating the public and seeking to prevent flooding of the U.S. with fentanyl and fentanyl-laced fake pills resembling Xanax, Oxycontin, Adderall, Vicodin and other popular prescription medications—but with a deadly twist. The counterfeit pills, more often than not, contain a lethal dose of fentanyl.
“CADCA and its 7,000 coalition members across the nation have worked tirelessly to address the issue of fentanyl-laced fake pills that are poisoning our nation’s youth by planning and implementing comprehensive, data-driven strategies, with multiple public and private partners to address community conditions causing this problem,” said CADCA’s president and CEO, retired Army general Barrye L. Price.
Across the country, fentanyl has largely fueled a more than doubling of overdose deaths among children ages 12-17 since the start of the pandemic. The deaths were inadvertently hidden by “good news” reported by the CDC on May 15, 2024, announcing that there were an estimated 107,543 drug overdose deaths in the U.S. during 2023—a decrease of 3% from the 111,029 deaths estimated in 2022.
Fentanyl is killing adolescents and people of color, many with no idea they are taking fentanyl. The counterfeit drugs are easy to obtain from friends or buy through social media. Sold online for $2 to $10 apiece, their lethal potency caught policy leaders, emergency rooms, addiction experts, family health providers, and pediatricians nationwide by surprise.
Such is the fentanyl crisis as of June 2024. As i will describe in this blog post, there are treatments of last resort and medications designed to reverse the effects of fentanyl when education, prevention, and treatment have failed. An estimated 80,000 deaths per year are attributed to opioid-induced respiratory depression (OIRD) caused by fentanyl alone. Wonder medicines that counter the effects include the widely-used naloxone (Narcan) and much-less-used (but also effective) opioid overdose reversal drug nalmefene (Opvee).
The Life-Saving Role of Naloxone
Naloxone has gained attention as a wonder drug capable of reviving a person who has overdosed, appeared to have died, or nearly died. I adminishtered, intravenously, my first dose of naloxone in 1975 while working in the Yale New Haven Hospital emergency room.. At the time, naloxone was most often given intravenously by anesthesiologists during surgery to reverse the sedative effects of opioids doctors had administered earlier. When naloxone was approved by the FDA in 1971, total drug overdose deaths in the U.S. were 6,771, rare enough that there was no national call to add it to emergency rooms to reverse overdoses. Since then, the number of overdoses has catastrophically escalated.
When Individuals Overdose on Opioids
What are signs of an opioid overdose? They include unconsciousness, very small eye pupils, slow or shallow breathing, vomiting, inability to speak, faint heartbeat, limp arms and legs, pale skin, and purple lips and fingernails. When a person overdoses on opioids, breathing slows or altogether stops. The overdosed person appears sleepy and is unresponsive.
Opioids
interfere with receptors in the brain, slowing breathing so that insufficient oxygen reaches the brain and other vital organs like the heart; the heart rate may slow or even stop. As breathing slows, oxygen levels fall, which may trigger abnormal heart rhythms. Blue lips and fingernails signal the lack of oxygen. Because insufficient oxygen reaches the brain and heart, the consequences are coma, brain damage, or death.
The antidote, naloxone, attaches to opioid receptors, reversing and blocking effects of opioids. Naloxone can quickly restore normal breathing. Naloxone is so safe we give it immediately to anyone with signs of opioid overdose or when an overdose is suspected. However, the drug has no effect on someone with no opioids in their system.
Reversing Respiratory Depression
The specific mechanism that drives opioid death by overdose is stimulation of one class of endogenous opioid receptors—mu-opioid receptors—in cells in the brainstem; it inhibits breathing. Respiratory depression, or decreased (or terminated) breathing, is a direct effect of opioid use, and, in the case of fentanyl, it appears extremely quickly.
Intravenous naloxone is not available in the community, where first responders depend on intranasal or intramuscular administration. Yet naloxone must be administered much sooner for fentanyl than for heroin because the window for saving the overdosed person is much shorter than with heroin. So, the right dose of naloxone must be given by a friend, loved one, or first responder almost immediately.
Other opioid antagonists, like nalmefene, may be expected to do a better job in fentanyl overdoses. After the person recovers, they should be offered long-term treatment resources, including the ability to initiate treatment for opioid use disorder in the emergency department, as Yale’s Brian Fuerhlein described in an earlier blog post.
Renarcotization
Researchers, addiction experts, and other healthcare providers have documented that when fentanyl is taken chronically, the drug may be absorbed into fat tissue and stay there, accumulating and forming a reservoir of fentanyl. Naloxone might reverse a “normal” fentanyl overdose, but due to the “depot effect,” after a person becomes conscious, they may lose consciousness again and stop breathing. This event is called re-narcotization.
If it is suspected that someone has overdosed on fentanyl and they are given naloxone, they may start breathing again and become conscious. With less potent opioids, naloxone can cover someone for 60 minutes. But someone with a supply of fentanyl in body fat depots can renarcotize several times. It is important to call 911. Additional doses of naloxone may be given as the patient is transported to the ER or hospital, where oxygen and other life support is available.
Narcan Nasal Spray
Naloxone can now be administered by non-health professionals via nasal spray to save lives. Intranasal naloxone works within two to three minutes. If the person has not responded after three minutes, another dose should be given. After administering naloxone, it’s very important to always call 911 because experts need to determine whether respiratory support, more naloxone, or other measures are necessary to reverse the overdose.
The FDA approved Narcan (naloxone) as a nasal spray for over-the-counter use because it is safe, easy to use, and saves lives. In 2021, the Food and Drug Administration approved an 8-mg intranasal naloxone product, twice the amount than the usual 4-mg dose. The FDA also granted a second over-the-counter naloxone agent in early 2024. This drug, RiVive, is a generic naloxone nasal spray available from Harm Reduction Therapeutics, a nonprofit pharmaceutical organization. Nasal naloxone is currently available in 3mg (Revive), 4mg (Narcan), and 8mg (Kloxxado) dosages.
Making naloxone available without a prescription expands its availability to people with an opioid-dependent loved one or who themselves have opioid use disorder (OUD). To save someone from an opioid overdose, you need naloxone or nalmefene. Steps for responding to an opioid overdose can be found here.
Another Opioid Overdose Reversal Drug: Nalmefene
Nalmefene has been saving lives from opioid overdoses since May 2023, when the FDA approved nalmefene hydrochloride nasal spray (Opvee). Nalmefene is a long-duration opioid antagonist first approved for injection in 1995. The original injectable nalmefene was removed from the market for commercial reasons in 2008. However, the dramatic rise in opioid overdose deaths and the emergence of powerful synthetic opioids catalyzed the development of an intranasal (IN) form of nalmefene for emergency treatment of opioid, and especially fentanyl, overdoses.
Nalmefene is an opioid receptor antagonist particularly well-suited for fentanyl overdoses. One reason is it has a longer half-life than naloxone, which means it stays in the body longer. This may protect against re-intoxication but may also make withdrawal symptoms last longer in those with opioid use disorders.
Synthetic opioids like fentanyl are now the most common drugs involved in drug overdose deaths in the U.S. Nalmefene is 10 times more potent than naloxone and has an 8- to 10-fold longer half-life (8 to 11 hours), reducing the likelihood of re-overdosing from long-acting opioids.
Xylazine and other adulterants illegally added to opioids in the U.S. have also received attention for generating zombie-like behavior in people. Such additives make overdose reversal more difficult. However, the key to harm reduction is reversing the effects of synthetic opioids on the heart, lungs, and brain.
The efficacy of frontline, community-based reversal of poisoning events with antidotes such as naloxone has been questioned due to the rise of highly potent synthetic opioids, primarily illicitly manufactured fentanyl (IMF), which causes 90% or more of opioid deaths in the U.S.
In many cases today, community-based first responders have improvised or evolved strategies to cope with fentanyl. Typically, multiple naloxone doses are given to individuals who overdosed on opioids. That was definitely not the case when I was giving naloxone to patients in the Yale emergency department in the 1970s or even back when the opioid crisis was primarily either a prescription-opioid or heroin crisis.
However, it’s unclear whether giving opioid overdose patients more doses sequentially is the optimal strategy in dealing with fentanyl. A very nice study by Strauss suggests it’s a good idea to have higher doses of intranasal naloxone available, as it appears that a large first dose at once is superior to the same dose given sequentially.
Some overdoses might be relatively naloxone-resistant and more easily respond to nalmefene. Additional research is needed to determine the optimal naloxone-dosing schedule for fentanyl overdose reversal. Multi-site studies directly comparing nalmefene to naloxone in the community setting are needed.
Conclusion
More than 1 in 8 Americans have had their lives disrupted by a drug overdose. Nearly 49 million Americans (more than 17%) age 12 and older have a substance use disorder. Among young adults aged 18-25, the share jumps to 28%. More than 6 million people had an opioid use disorder, and another 1.8 million had a methamphetamine use disorder in 2022.
The evolving opioid epidemic has morphed into a counterfeit-pill, multi-drug crisis centered on fentanyl, often paired—knowingly or unknowingly—with other illicit drugs. Smoking fentanyl is the newest opioid crisis or problem we have not prevented.
Overdose deaths are only one measure of the drug epidemic's severity. An estimated 321,566 children lost a parent to drug overdose between 2011 and 2021.
Since 2000, more than 1.1 million overdose deaths have been reported in the U.S. Overdose reversal with intranasal anti-opioids like naloxone and nalmefene has made a big difference but should not be the centerpiece of opioid crisis strategy. Education and prevention are needed and, as we develop new and better treatments for OUDs, so are overdose reversal and relapse prevention. Some very effective means to reverse opioid overdoses are available today, and future research should provide further information on the best medication and dosages for fentanyl overdose situations.
References
Skolnick P. On the front lines of the opioid epidemic: Rescue by naloxone. Eur J Pharmacol. 2018 Sep 15;835:147-153. doi: 10.1016/j.ejphar.2018.08.004. Epub 2018 Aug 7. PMID: 30092179.
Ellison M, Hutton E, Webster L, Skolnick P. Reversal of Opioid-Induced Respiratory Depression in Healthy Volunteers: Comparison of Intranasal Nalmefene and Intranasal Naloxone. J Clin Pharmacol. 2024 Mar 4. doi: 10.1002/jcph.2421. Epub ahead of print. PMID: 38436495.
Crystal R, Ellison M, Purdon C, Skolnick P. Pharmacokinetic Properties of an FDA-approved Intranasal Nalmefene Formulation for the Treatment of Opioid Overdose. Clin Pharmacol Drug Dev. 2024 Jan;13(1):58-69. doi: 10.1002/cpdd.1312. Epub 2023 Jul 27. PMID: 37496452; PMCID: PMC1081801
Stolbach AI, Mazer-Amirshahi M, Nelson LS, Cole JB. American College of Medical Toxicology and the American Academy of Clinical Toxicology Position Statement: Nalmefene Should Not Replace Naloxone as the Primary Opioid Antidote at This Time. J Med Toxicol. 2024 Jan;20(1):64-67. doi: 10.1007/s13181-023-00981-z. Epub 2023 Nov 30. Erratum in: J Med Toxicol. 2023 Dec 28;: PMID: 38032431; PMCID: PMC10774510.